- Find a Provider
-
Services
-
Redeemer Health provides compassionate care across every stage of life.
- View all Services
-
- Patients & Visitors
- Locations
- Careers
categories:

MEADOWBROOK, Pa. – November 2022 – Redeemer Health launched the first Hospital at Home program in the Philadelphia region this year. The program puts care providers in patients’ homes, delivering hospital-level acute care for patients with diagnoses such as pneumonia, urinary tract infection, cellulitis, dehydration, congestive heart failure, COPD and more. The Centers for Medicare & Medicaid Services (CMS) has approved 114 health systems to operate Hospital at Home programs so far, with five other systems approved in Pennsylvania.
“This is the future,” said Mary Ellen Cockerham, DNP, RN, senior director for Acute Care in the Home, who is heading the program’s launch. “This type of care can be done in the home safely, and it’s better for patients.” A national study of the Hospital at Home model found it to result in better clinical outcomes, higher patient and family satisfaction, fewer complications often associated with hospital stays, and less expense, she said.
The Hospital at Home program was recently granted $100,000 to purchase necessary in-home patient monitoring equipment and to outfit a command center at Holy Redeemer Hospital.
Patients enter the program from either Holy Redeemer Hospital’s emergency department or an inpatient unit, Cockerham explained. A physician provides ongoing assessment and treatment through a combination of in-home and virtual visits, along with a dedicated team of experienced RNs and health navigators. The program includes multiple daily visits, 24/7 access to on-call providers, transportation to and from Holy Redeemer Hospital, delivery of medication, equipment and three meals a day; and support from social workers, pastoral care, physical therapists and others.
To qualify, patients must meet criteria including safety of their home environment, family support and proximity to the hospital. Redeemer Health’s Hospital at Home program can accommodate traditional Medicare and Aetna Medicare patients. Additional coverage plans could be added soon.
Patients wear a “biovitals” patch that communicates their vitals and other information to a user-friendly electronic tablet they keep with them. The information is then sent to a command center at the hospital. Cockerham emphasizes that patients don’t need to be tech savvy to use the equipment, and internet access isn’t necessary. “The equipment is very easy to use, even for those who are not comfortable with computer equipment,” she explained. “For example, one touch on the tablet screen can request a nurse call, visit, or telehealth appointment.”
She notes that while Hospital at Home is new to the Philadelphia region, the concept is well-established. “The pandemic certainly was a catalyst for Hospital at Home,” she says. “But the concept has been around since the 1970s. Other countries are using it with success.” American health systems that have adopted the model include Duke Health, Cleveland Clinic, Mount Sinai Health System, Brigham and Women’s Hospital, Massachusetts General Hospital, the Mayo Clinic, and Geisinger Medical Center in central Pennsylvania.
categories:

MEADOWBROOK, Pa. – October 2022 – A new technology at Redeemer Health is helping reduce or even avoid lymphedema, nerve injury, and shoulder mobility issues in some mastectomy patients. These improved outcomes in patients with breast cancer result from leaving lymph nodes intact during surgery.
The new localization system harnesses the power of magnetics to guide decisions. Its probe works like a metal detector that, when placed near the skin, detects magnetic markers that help determine the scope of breast and lymph node surgery.
This option is particularly relevant for those with an early form of breast cancer called ductal carcinoma in situ, or DCIS, who are undergoing mastectomy. It has normally been the practice with such patients to remove sentinel lymph nodes at the time of surgery in case the cancer is invasive and has spread to those nodes. Sentinel lymph nodes are the first lymph nodes to which cancer cells are likely to spread from a primary tumor. Their removal is typically critical in determining whether a breast cancer has spread and helps set a course of treatment.
“It has a lot of advantages,” says Dr. Stacy Krisher, breast surgeon and medical director of the breast health program at Redeemer Health in partnership with MD Anderson Cancer Center at Cooper. “This is a step forward in the surgical treatment of breast cancer.”
Dr. Krisher explains that traditionally dye mixed with radioactive material is injected into the breast to identify the sentinel lymph nodes for removal. The dye is picked up by the breast’s lymphatic system and travels through the lymphatic vessels to the lymph nodes in the patient’s armpit. When using conventional dyes, which stay in the nodes for only a couple of hours to a day, the lymph nodes must be taken out right away.
This system, on the other hand, enables a process called delayed sentinel lymph node biopsy. A liquid tracer that has been developed specifically for sentinel node biopsies is injected before the mastectomy, and because it remains in the lymph nodes for up to 30 days, there is time to get a pathology report on the breast and determine whether sentinel lymph node removal is necessary. If the cancer is deemed non-invasive, patients can safely keep their lymph nodes. But if there’s concern that the cancer has spread, the tracer dye will still be in the sentinel nodes to guide a biopsy.
According to the system manufacturer, up to 80% of ductal carcinoma in situ (DCIS) patients do not need to have their lymph nodes removed. Leaving the nodes intact spares these patients the potential negative effects of lymph node removal, such as a fluid build-up called lymphedema.
“There are a lot of potential side effects to removing lymph nodes,” says Dr. Krisher. “It can cause lymphedema in the arm or chest wall that can be problematic and can increase the risk of having numbness. Any surgery in the axilla can further affect arm movement or extend recovery.”
The longer time frame provided by this system is critical, she says. “If we do find invasive cancer, we go back and take the lymph nodes if we need to. But we can otherwise leave them in place and avoid the risks of lymphedema, nerve injury, and shoulder mobility issues.”
Dr. Krisher has had cases in which the lymph nodes would automatically have been removed, but thanks to the new system they were preserved.
Additionally, the system provides a new way to target tumors for removal that improves comfort and convenience for patients. The magnetic marker is used to localize tumors, helping surgeons to accurately detect and remove it.
topics in this article
categories:

MEADOWBROOK, Pa. – November 2022 – St. Joseph Manor has earned its place on Newsweek’s Best Nursing Homes list again. The 2023 list recognizes 475 nursing homes in 25 states, only two of which are in Montgomery County, Pa.
“The indicators ranking nursing homes in this survey validate what we’ve known about St. Joseph Manor all along,” said Christine Holt, Executive Vice President and COO of Life Care at Redeemer Health. “We provide not only comprehensive long-term care, but also a full range of amenities that enrich the lives of our residents. We are so proud that we’ve earned this distinction for two years in a row, because it signifies that treating our residents like family creates a legacy of high quality service.”
St. Joseph Manor provides both long- and short-term care. In addition to long-term, individualized care for residents, caregivers provide short-term services that help prepare patients for a safe return home after a hospital stay. These include physical, occupational and speech therapy, wound care, infusion, nutrition counseling, social services, and many physician specialties.
The Best Nursing Homes 2023 ranking lists facilities with excellent key performance data, peer recommendations, accreditation, and response to the COVID-19 pandemic.
St. Joseph Manor is located at 1616 Huntingdon Pike, in Meadowbrook, Pa. Call 215-938-4108 or visit here to learn more. For more information about Redeemer Health’s Life Care communities, visit here.
categories:

MEADOWBROOK, Pa. – Nov. 16, 2022 – Holy Redeemer Hospital received an “A” grade for hospital safety for the seventh time in a row from the Leapfrog Group. The fall 2022 grade reveals high achievements in infection prevention, handwashing and safe medication administration. The hospital has scored an “A” every semiannual cycle since fall 2019.
“Some of our high scores in this cycle’s survey have to do with staff working together to enforce safety, effective leadership in prevention of errors, and the qualifications of our nurses and ICU physicians,” said William Scarlett, DO, MHCM, FACS, FACOS, Senior Vice President Cancer Care and Health Care Delivery at Redeemer Health. “High performance in those talent-based categories results in excellent scores across the board. We’re proud of our team for its ongoing commitment to patient safety.”
The Leapfrog Group, an independent national organization, assigns letter grades to hospitals across the country based on more than 30 performance measures reflecting errors, accidents, injuries and infections, as well as the systems hospitals have in place to prevent harm. According to the Leapfrog Group, its hospital safety grade is the only ratings program based exclusively on hospital prevention of medical errors and harm to patients. The grading system is peer-reviewed, fully transparent and free to the public. An “A” is a sign that hospitals are continuously evaluating their performance, so that they can best protect patients, according to the Leapfrog Group.
“Our continued success in safe patient care is a reflection of the commitment we made years ago and continue to live up to,” said Jeanette Teets, Redeemer Health VP and Chief Quality, Safety and Reliability Officer. “This level of ongoing success requires focus and responsiveness from all caregivers, staff and leadership.”
To see Holy Redeemer’s grade details and to access patient tips for staying safe in hospitals, visit HospitalSafetyGrade.org.
categories:

Through its special “We Honor Veterans” program, Redeemer Health Hospice brings inspiring bedside tributes to patients who are former service members.
“Honoring veterans—especially at the end of life—is an honor and a privilege,” says Hospice Clinical Manager Dana Clemons. “Many of our clinicians, including myself, are family members of veterans. Participating in the We Honor Veterans program provides a way for us to respect and serve those who gave to our country.”
One moving tribute came to Ernie*, a 97-year-old World War II Veteran under the care of Redeemer Health Hospice. A nurse learned that when Ernie was deployed to Italy and stationed with his regimen to a hill the Germans occupied, our country was losing the war. Ernie threw a grenade that blew up the hill, but in exchange, the Germans returned a grenade that landed on his abdomen. Ernie was the sole survivor from his regimen.
Grateful to Ernie and all others who sacrifice for their country, the hospice nurse arranged to honor Ernie through the We Honor Veterans program. A team was gathered to present Ernie with a veteran’s certificate, a patriotic blanket, and pin. During the pinning ceremony, a priest anointed Ernie with the sacrament of the sick.
These heartfelt gestures meant the world to Ernie and his family—as it does to the many other veterans we have the privilege to serve.
Redeemer Health Hospice is honored to collaborate with the National Hospice and Palliative Care Organization and the Department of Veterans Affairs in offering the We Honor Veterans program. As a health care system that practices a holistic approach to patient care, we are proud to support the physical, emotional, and spiritual health of the beloved and time-honored veterans who entrust us with their care. Learn more about Redeemer Health Hospice or call 888-678-8678.
*Fictitious name is being used to preserve patient privacy.
categories:

“I’m so proud of Holy Redeemer Hospital and the entire system, for what you do for the youngest babies, for our seniors, and for everybody in between,” said Congresswoman Madeleine Dean during a roundtable discussion about maternal health at Holy Redeemer Hospital. “When it comes to addressing health needs, the pandemic underscored the health disparities in our nation, with poor and minority populations in the greatest need. Yet, they are often ignored and left in the shadows. Not here at Holy Redeemer.”
Redeemer Health proudly hosted the discussion and a tour of the NICU with Rep. Dean and Xavier Becerra, U.S. Secretary of the Department of Health and Human Services. Dr. Ala Stanford, Regional Director of the Department of Health and Human Services also joined. Redeemer Health hosts included Holy Redeemer Hospital’s Chief Administrative Officer, Cass Egan; Chief Nursing Officer, Anne Catino; and Director of Maternal Child Health, Christina Marczak. Other guests included fellow grant awardees Martha Sharkey, founder of Today is a Good Day Foundation; and Dr. Alberto Esquenazi, Chief Medical Officer at MossRehab.
The goal of the visit was to talk with our hospital leaders about maternal health programs, specifically services for new mothers who are challenged with addiction.
“President Biden has instructed us to invest directly in maternal health,” said Secretary Becerra. The Redeemer Health programs serving moms struggling with addiction recently were awarded two grants to fund program expansion.
Critical services for pregnant mothers with substance use disorder (SUD) and their babies who are born with neonatal abstinence syndrome (NAS) expanded thanks to the grants. One of the grants was awarded by United States Substance Abuse and Mental Health Services Administration, and the other came thanks to Rep. Dean’s support via congressionally directed funding. The number of babies born with NAS in the Philadelphia region has increased significantly in recent years, so this expansion is vital to the Redeemer Health mission.
The hospital’s SUD program works to improve outcomes for mothers with addiction since 2013. Historically, treatment has included psychosocial care and clinical support. With the grant funds, Redeemer Health added an initiative called Navigational Empathy for SUD and Treatment (NEST), providing additional access to behavioral health counseling services and support from patient navigators.
“The opioid epidemic in the Philadelphia region has put so many moms and babies at risk,” said Catino. “The funding gave us the capacity to support these patients with a trusted advocate who provides resources that strengthen their well-being. We now provide the services of a behavioral health counselor who offers in-person and telehealth services to these vulnerable patients.”
NEST navigators eliminate barriers to transportation, appointment scheduling, counseling and childcare. They connect patients with dietary consultants, parenting education and childbirth classes, early intervention services for non-insured families, recovery support activities, and translation support for patients whose language of choice is not English.
About 40 families affected by SUD and NAS are cared for at Redeemer Health every year, said Catino.
Photo - During a discussion with dignitaries about maternal health at Redeemer Health, clockwise from left: Dr. Alberto Esquenazi, Martha Sharkey, Dr. Ala Stanford, Sec. Xavier Becerra, Rep. Madeleine Dean, Cass Egan, Anne Catino, and Christina Marczak, MSN, RN.
categories:

If you’re a wartime veteran or the surviving spouse of a veteran who needs supportive care, you should know about a VA program that can help pay for that care.
The Aid and Attendance Pension, a benefit of the Department of Veterans Affairs, provides monthly income to veterans and their surviving spouses to help pay for an assisted living or personal care facility, home care provider, adult day center, or nursing home.
The program supports veterans who require care for a disability unrelated to their military service or need help with daily living activities. The VA will also provide income to a surviving spouse who was married to a veteran with qualifying military service. Eligibility is based on the veteran’s wartime service, health and care needs, income versus medical expenses, and total assets. In 2023, benefit will pay $1,432-$2,642 per month, tax-free.
A free webinar about the benefit, sponsored by Redeemer Health, took place on November 10, led by Emily Schwarz, President of AidandAttendance.com. You can view a video of the webinar here.
“A lot of veterans and surviving spouses don’t realize this program is available to help pay for assistance with care and activities of daily living,” says David McDonald, Personal Care Administrator for Redeemer Health. He notes that Redeemer Health offers two communities—in Northeast Philadelphia and Montgomery County—that accept the payments.
Who is Eligible?
AidandAttendance.com provides a short, free evaluation tool you can use to see if you meet eligibility criteria and are a good candidate to apply. More information on criteria and applying for the benefit are available at AidandAttendance.com.
Qualifying wartime military service includes:
- World War II
- The Korean Conflict
- Vietnam Era
- Gulf War
Types of care expenses that qualify include:
- Assisted living or personal care
- Home care
- Senior living (with care)
- Memory care
- Adult day care
- Nursing home
More information on the program is available by calling AidandAttendance.com at 800-626-7145 or the VA at 800-827-1000.
A Local Opportunity
Redeemer Health’s communities for older adults are among the facilities that qualify to accept the VA Aid and Attendance benefit. These communities help older adults stay safe and independent while enjoying access to therapeutic, social, recreational, and spiritual life opportunities.
Redeemer Health Lafayette in Northeast Philadelphia, and St. Joseph Manor in Meadowbrook, PA, offer personal care accommodations and services that include:
- A wide range of personal care apartments, suites, and rooms to suit many preferences and budgets
- Housekeeping and linen services
- Three meals daily
- Recreational programs
- Pastoral care
- Nightly check-in by nursing staff
- Assistance with medical appointment scheduling, medication management, dressing, washing and grooming
If residents' care needs should increase, the communities offer additional assistance via progressive levels of personal care.
Residents enjoy additional peace of mind knowing that the facilities' unique status as members of the Redeemer Health family gives them access to Redeemer Health's wide-ranging expertise and resources.
For more information on Redeemer Health's communities, visit redeemerhealth.org/lifecare/personal-care or call 215-214-2877.
categories:
I Believe in Hope
After Rosemarie Sulock's son was shot in the thigh while on duty as a Philadelphia police officer, she quickly lost 25 pounds. She thought it was due to stress.
Then her son's friend visited and, shocked by how thin Rosemarie looked, asked whether she had cancer.
Rosemarie thought about that conversation when she visited her gynecologist. Soon after, she noticed a round, stone-like object in her chest wall and, because she "knew her body," she asked for a mammogram.
She scheduled her mammogram with Anna Mazor, DO, breast surgeon with Redeemer Health in partnership with MD Anderson Cancer Center at Cooper. Dr. Mazor also performed an ultrasound.
Rosemarie said Dr. Mazor's pleasant demeanor put her at ease. "I just felt connected to her right away," Rosemarie said. "I felt like she was a friend I hadn't seen in a couple of years."
The ultrasound detected the object Rosemarie had noticed. Dr. Mazor immediately removed the small mass and used a fine needle to check for cancer cells.
Test results showed that Rosemarie had invasive ductal carcinoma, a type of breast cancer. Dr. Mazor recommended that Rosemarie have a lumpectomy, rather than a mastectomy, because they caught the cancer early.
As Rosemarie considered what to do, she mulled opinions from family members. She also was concerned about the timing, with her daughter's wedding coming up in a few months.
"I needed peace in my heart," Rosemarie said. So she went to the Healing Consciousness Foundation, a Redeemer Health affiliation which helps people affected by breast cancer improve their quality of life through education, lifestyle modification, and holistic healing.
Rosemarie chose to have the lumpectomy. During the procedure, Dr. Mazor also removed three lymph nodes. One turned out to be cancerous.
After her lumpectomy, Rosemarie needed radiation treatment. Under the care of radiation oncologist Sheena K. Jain, MD, Rosemarie received 32 radiation sessions. Still working, she traveled to her appointments during her lunch breaks.
Rosemarie finished treatment on Oct. 10, 2019 - "the happiest day of my life," she said. Following patient tradition, she rang a bell, which signified the end of her cancer treatment. Afterward, she ordered pizzas, hoagies "and all kinds of goodies" for the staff and gave them cards thanking them for pulling her through her cancer treatment.
"They were just so compassionate, patient, and loving," she said.
 She had a little time to recuperate before flying to Arizona for her daughter's November wedding. When she returned home, Rosemarie had contracted lymphedema, a non-lethal, but painful side-effect that some patients experience after cancer treatment. She had swelling and cording down her arm, which made her arm difficult to move. Dr. Mazor started her on eight months of physical therapy, including exercises Rosemarie did at home.
She had a little time to recuperate before flying to Arizona for her daughter's November wedding. When she returned home, Rosemarie had contracted lymphedema, a non-lethal, but painful side-effect that some patients experience after cancer treatment. She had swelling and cording down her arm, which made her arm difficult to move. Dr. Mazor started her on eight months of physical therapy, including exercises Rosemarie did at home.
Then in February 2020, Rosemarie learned that her breast cancer had returned. Out of caution, she sought a second opinion from another doctor, who confirmed Dr. Mazor's diagnosis of invasive mammary tubular carcinoma. Rosemarie returned to Dr. Mazor for another lumpectomy.
"I just love Dr. Anna," Rosemarie said.
Rosemarie noted that the receptionists at the doctors' offices were helpful. She also singled out for praise the nurse navigators in Dr. Mazor's office, who would call to check on her every few days. "Sometimes I cried on the phone with them," Rosemarie said. "I said, 'I feel like you guys are my family.'"
After the second surgery, Rosemarie underwent 21 radiation sessions. Unlike her first round of radiation, this time Rosemarie couldn't bring family or friends with her because of the COVID-19 pandemic. Staff kept her company, inquiring about her six grandchildren, including two sets of twins, and asking about the details of her daughter's wedding the previous year.
Today, Rosemarie is doing well. She now routinely sees hematologist and oncologist Pallav K. Mehta, MD for follow up care. She expects to see him for 10 years.
Rosemarie has gained back the weight she lost. In April, she turned 61. That same month, she had another mammogram. "Everything is clear," she said.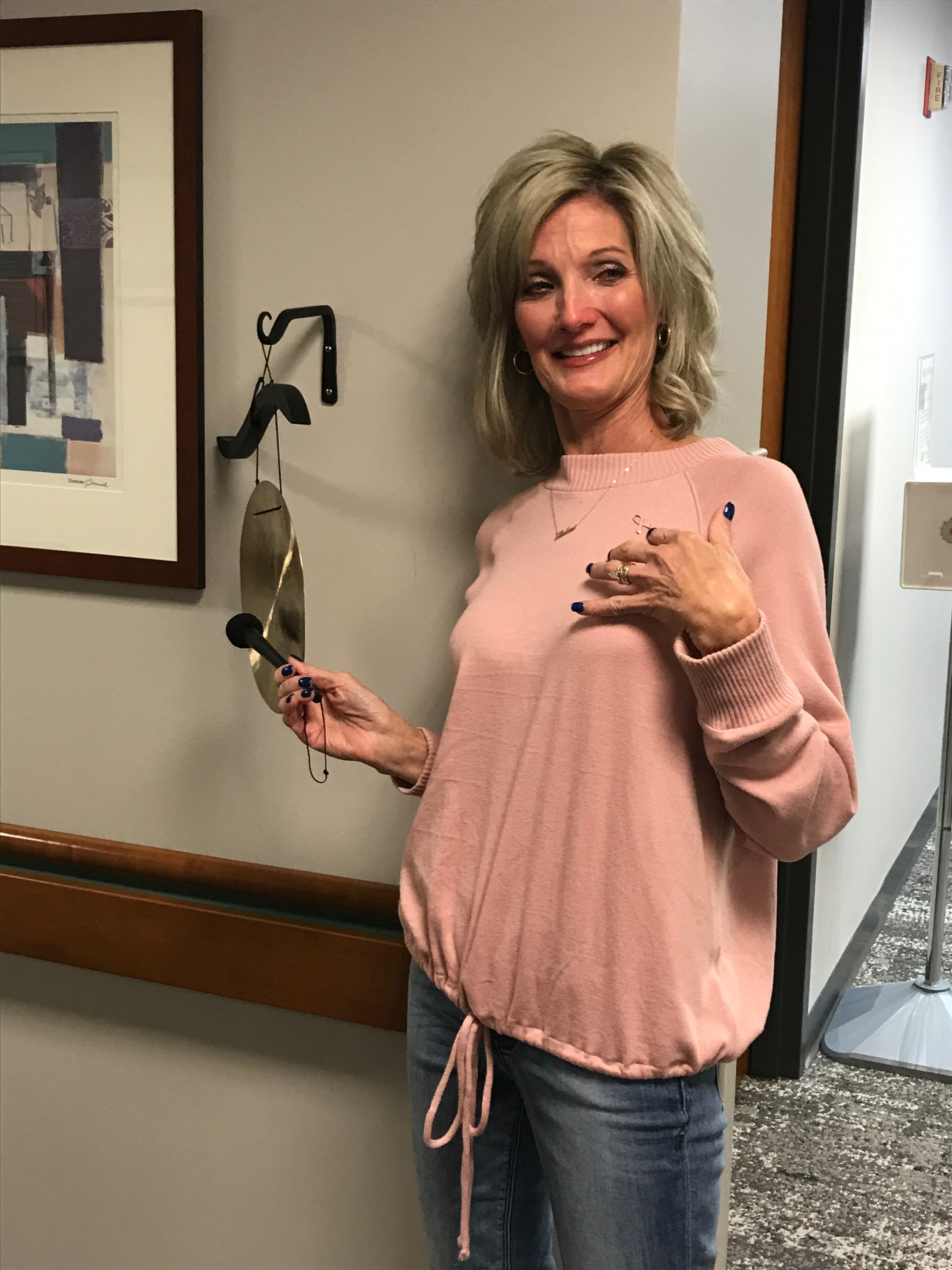
Rosemarie couldn't thank doctors and staff enough for their dedication and kindness, and for helping her to stay strong throughout her treatments.
"I believe in hope," she said. "I know the doctors at Redeemer Health in partnership with MD Anderson at Cooper all made me feel hope, and I continue to have hope for all those who are now going through cancer treatment."
Learn more about breast cancer services at Redeemer Health in partnership with
MD Anderson at Cooper.
