- Find a Provider
-
Services
-
Redeemer Health provides compassionate care across every stage of life.
- View all Services
-
- Patients & Visitors
- Locations
- Careers
categories:
Redeemer Health Maternity is here with you throughout your most precious journey. From planning to become pregnant, to post-delivery, and beyond - our team of dedicated, experienced professionals are available to assist. We've heard from a few moms who shared their experiences and offered words of advice to expecting moms!
 Farah, Mom and baby girl Suhani
Farah, Mom and baby girl Suhani
"I had the best experience at Redeemer Health - my doctor, nurses and all the staff there are so friendly, supportive, and professional. They were always ready to help me and my husband. Ask as many questions as you want to ask and just relax because you are in good hands."
Jess, Mom of 3 - Makenzie, Ryan and Nolan
"My experience at Redeemer Health each time was very different.  I had a natural birth, an induced birth and the grand finale, an emergency C-section. The nurses treated me like I was a friend they've known forever. They made sure I was always comfortable and always answered any question I had. My favorite part of being a Redeemer Mom is the connections I made with the nurses. While being in the NICU with my third, they became my family. I love being able to randomly text them pictures of my kids and catch up with them. They genuinely care about you!
I had a natural birth, an induced birth and the grand finale, an emergency C-section. The nurses treated me like I was a friend they've known forever. They made sure I was always comfortable and always answered any question I had. My favorite part of being a Redeemer Mom is the connections I made with the nurses. While being in the NICU with my third, they became my family. I love being able to randomly text them pictures of my kids and catch up with them. They genuinely care about you!
A tip I would pass on to another Redeemer Mom - take the picture. Life flies by so fast, take pictures with your kids, of your kids, and create memories they will forever remember."
Amanda, Mom and baby boy Averi
 "My experience at Redeemer Health was honestly amazing! I had high blood pressure during the end of my pregnancy and needed to be induced. I got a room at 11 p.m. and gave birth around noon the next day! Through it all the nurses were so supportive and encouraging! They answered all the questions I had, and as a first time mom I had quite a few! My favorite part of being a Redeemer Mom is the community and experiences we're all able to share, and the advice!"
"My experience at Redeemer Health was honestly amazing! I had high blood pressure during the end of my pregnancy and needed to be induced. I got a room at 11 p.m. and gave birth around noon the next day! Through it all the nurses were so supportive and encouraging! They answered all the questions I had, and as a first time mom I had quite a few! My favorite part of being a Redeemer Mom is the community and experiences we're all able to share, and the advice!"
Keychla, Mom of 3 - Amari, Anthony and Aura
"My experience at Redeemer Health was amazing every time. I love how friendly all the nurses are and how I felt heard and cared for without judgement every time. I always tell everyone to go to Redeemer Health! My favorite part of being a Redeemer Mom is knowing that my children and I are always cared for whenever we walk through those doors! I would tell other Redeemer Moms to have faith that everything will turn out exactly the way it needs to, and to always trust your gut and ask questions. The nurses/doctors will answer every question with their best ability."
would tell other Redeemer Moms to have faith that everything will turn out exactly the way it needs to, and to always trust your gut and ask questions. The nurses/doctors will answer every question with their best ability."
To find an OB/GYN or to learn more about our maternity services, please visit us at redeemerhealth.org/maternity. Want to join our community or share your maternity story? Please join us at @Redeemerbaby on Facebook or Instagram.
categories:

Redeemer Health in partnership with MD Anderson Cancer Center at Cooper earned a three-year accreditation from the Commission on Cancer, a quality program affiliated with the American College of Surgeons. Qualifying for “Comprehensive Community Cancer Program” accreditation means it meets 34 quality care standards and maintain levels of excellence in the delivery of comprehensive patient-centered care.
Accreditation provides focus on quality for cancer prevention, early diagnosis, cancer staging, optimal treatment, rehabilitation, life-long follow-up for recurrent disease, and end-of-life care, explained William Scarlett, DO, Sr. VP of Cancer Care at Redeemer Health in partnership with MD Anderson at Cooper, and Medical Director of Health Care Delivery at Holy Redeemer Hospital. “As an accredited center, we take a multidisciplinary approach to treating cancer as a complex group of diseases that requires consultation among surgeons, medical and radiation oncologists, diagnostic radiologists, pathologists, and other cancer specialists. This multidisciplinary partnership results in improved patient care,” he said.
This achievement also gives patients access to information about clinical trials and new treatments. Included are genetic counseling, psycho-social support, a patient navigation process, and a survivorship care plan that documents the care each patient receives.
topics in this article
categories:

Stroke is a serious and often life-threatening medical emergency that happens when the blood flow to the brain is interrupted. According to the American Heart Association, approximately 795,000 people in the U.S. suffer from a stroke every year, and every 3.5 minutes, one person dies from a stroke.
Approximately 80% of all strokes are caused by lifestyle choices.
Keep reading to learn more about the warning signs and risk factors for stroke, as well as dietary changes and other steps you can take to help reduce your risk.
Know the Warning Signs
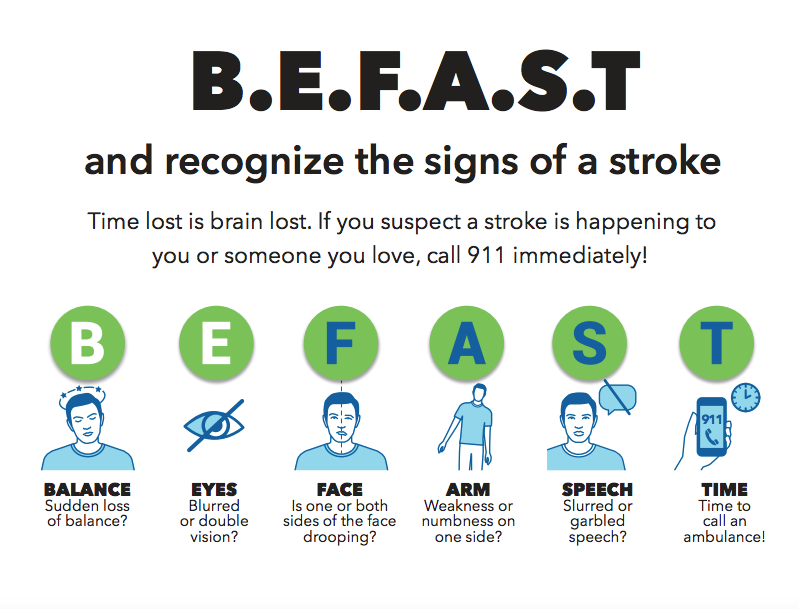
Every second counts when it comes to treating a stroke. Early intervention can prevent permanent brain damage and other complications. If you suspect a stroke is happening to you or someone you love, call 911 immediately.
Look at the time of onset and use the B.E.F.A.S.T. test (below) to help remember the warning signs of stroke:
Know the Risk Factors
Risk factors for stroke include high blood pressure, smoking, diabetes, high cholesterol levels, obesity, physical inactivity, family history of stroke, and age (those over age 55 have a higher risk).
Other factors that may increase the likelihood of stroke include atrial fibrillation, previous stroke or transient ischemic attack (TIA), certain medical conditions such as sickle cell disease, and the use of certain medications.*
*The benefits of certain medications may outweigh the potential risks. Always follow your doctor's advice regarding medication changes or adjustments.
A Healthy Diet and Physical Activity Can Lower Your Risk
Eating a healthy diet and making healthy choices, such as choosing fruits and vegetables, limiting processed and high-fat foods, and limiting alcohol consumption, can help lower your risk of stroke.
In addition, being active for a minimum of 30 minutes every day can help control blood pressure, increase good cholesterol, and make your heart stronger. Physical activity also makes your blood vessels more flexible and reduces the chance of having a stroke.
Making Small Changes Now is Worth it for a Lifetime of Better Health Later!
Not only during Stroke Awareness Month, but all year long – make your health a priority. A healthy lifestyle not only promotes overall well-being and improves quality of life, but it can also be life-saving.
Talk to your doctor about lifestyle choices that can help prevent stroke from happening in the future.
To find a Redeemer Health family doctor or primary care physician, visit the Redeemer Health website.
categories:

MEADOWBROOK, Pa. – May. 3, 2023 – Holy Redeemer Hospital received an “A” grade for hospital safety for the eighth time in a row from the Leapfrog Group. The spring 2023 grade reveals high achievements in staff and leadership working together to prevent errors, communication with nurses, and safe medication administration. The hospital has scored an “A” every semiannual cycle since fall 2019.
According to the Leapfrog Group, Holy Redeemer Hospital is among only 29% of hospitals nationwide to achieve an "A" grade this spring. There were only 59 hospitals to achieve an "A" in Pennsylvania. Scores are based on more than 30 national performance measures reflecting errors, accidents, injuries, infections, and harm prevention.
“At the national level, we saw deterioration in patient safety with the pandemic,” said Leah Binder, president and CEO of The Leapfrog Group. “But this hospital received an ‘A’ despite those challenges. I congratulate all the leaders, staff, volunteers and clinicians who together made that possible.”
According to William Scarlett, DO, MHCM, FACS, FACOS, Senior Vice President Cancer Care and Health Care Delivery at Redeemer Health, “Maintaining high scores in error prevention and medication administration over a long period of time reflects a culture of safety. This reveals the ongoing commitment made by every teammate in our hospital.”
The Leapfrog Group, an independent national organization, assigns letter grades to hospitals across the country based on more than 30 performance measures reflecting errors, accidents, injuries and infections, as well as the systems hospitals have in place to prevent harm. According to the Leapfrog Group, its hospital safety grade is the only ratings program based exclusively on hospital prevention of medical errors and harm to patients. The grading system is peer-reviewed, fully transparent and free to the public. An “A” is a sign that hospitals are continuously evaluating their performance, so that they can best protect patients, according to the Leapfrog Group.
“Our continued success in patient safety is celebrated at Redeemer Health,” said Jeanette Teets, VP and Chief Quality, Safety and Reliability Officer. “This level of high performance is evidence of our focus and responsiveness from everyone, every day.”
categories:

Moving into a senior living community apartment is a great way to enjoy the rewards of retirement. From having access to social activities and amenities, to gaining peace of mind knowing there is help nearby if needed, seniors who make the move are often surprised by just how much they love and benefit from their new home.
Enjoying Companionship
Making friends contributes to our well-being. Seniors who live at a senior living community can connect with peers who have similar interests through various fun activities like art, games, and fitness programs.
Boosting Wellness
Senior living communities can help to foster better physical and mental health for residents. On-site medical care is readily accessible, in addition to fitness centers and classes promoting a healthy lifestyle. Residents enjoy staying active, engaged, socializing with peers, and staying independent for longer.
Gaining Peace of Mind
Many senior living communities have secure entrances and staff available day and night. Additional features like emergency call buttons, ramps, elevators, and grab bars provide extra peace of mind for residents and their families. Some communities also offer transportation services to residents for nearby shopping and doctor’s appointments. These features ensure safety and comfort to all residents.
Eliminating Home Maintenance and Its Costs
Senior living communities typically offer fixed monthly fees that include a wide range of services and amenities. This can be a huge relief for seniors who are tired of managing multiple bills and expenses each month. In addition, moving into a senior living community means there are no more home maintenance costs—which can be a large expense for seniors who live in homes that require frequent upkeep and repairs. Residents can enjoy greater security knowing their home is kept up-to-date with no additional effort or cost required!
Enjoying a Worry-free Lifestyle
Moving into a senior living community can be a very rewarding experience. With so much provided under one roof, residents can enjoy more time doing what they love. Additionally, the sense of security and fellowship provided by being part of a larger community is priceless.
Ultimately, a senior living community offers many benefits that can help enhance life during retirement, making it a sensible and worthy choice to consider.
It's All Right Here at Lafayette
A Redeemer Health senior living community, Lafayette offers all of the benefits described in this article—and more!
The community is located in Fox Chase, a neighborhood featuring tree-lined streets and beautiful green spaces. In fact, one of the many perks of living at Lafayette is the stunning views of Pennypack Park that residents can enjoy year-round.
Lafayette offers stylish, newly renovated apartments and a lively social atmosphere with a full calendar of activities, programs, and events. In addition, the community takes care of chores like housekeeping and linen service while offering many on-site conveniences such as a country store, bank, beauty salon/barber shop, and health care services.
Lafayette is perfect for seniors who want a worry-free lifestyle. Learn more today! Schedule a tour or speak with a residential sales coordinator now. Call 215-214-5877 or visit redeemerhealth.org/LafayetteLiving.
categories:

The earliest generation of Redeemer Health caregivers were our founding Sisters, who came to America to care, comfort, and heal the sick and poor in their homes. We are still answering that calling today, with nurses, therapists and home health aides following the compassionate example set by the Sisters nearly 100 years ago.
Our skilled professionals bring comfort, compassion, safety, and trust to each family we serve—all in the comforts of your own home. With our services, you will find nurses, therapists, and home health aides who provide skilled nursing, disease and pain management, wound care, and rehabilitative services. The key is knowing what type of home care to ask your doctor about. Here’s a quick tutorial:
- Home Care - Ongoing skilled care for chronic conditions that are manageable but improvement or recovery may be limited.
- Advanced Care at Home - Skilled and specialized care with a focus on quality of life and symptom management for patients who have advanced-stage illnesses that are not expected to improve.
- Support at Home - Assistance with daily living tasks, such as medication management, transportation, meal preparation, and companionship.
- Hospice Care - Once curative treatment has stopped for patients with a life-limiting illness, the focus shifts to comfort care and symptom management, support for patient and family, and quality at the end of life.
- Palliative Care - This provides you and your loved ones with extra support to lessen the burden of chronic or terminal illnesses. You can learn more about the difference between palliative and hospice care here.
Wherever you choose to get your home care services, be sure they focus on your overall health, medical history, abilities, lifestyle, goals, and other factors—all the things that make each patient unique. Now that you’re better informed, do you believe home care or hospice care can help you or a loved one? We’re happy to answer your questions. Please call 888-678-8678 or read more here.
categories:

Did you know that colorectal cancer is the third most commonly diagnosed type of cancer in both men and women over 45? Knowing the facts about early diagnosis and treatment, as well having conversations with your family or primary care doctor about screenings, are two important steps you can take to help reduce risk.
Tips to lower your risk
Living a healthy lifestyle can help decrease your chances of developing colorectal cancer. This includes taking steps like:
- Maintaining a healthy weight
- Avoiding smoking
- Limiting alcohol consumption
- Engaging in regular physical activity
- Maintaining a balanced diet that includes lots of fresh fruits, vegetables and whole grains, while limiting processed meats
Additionally, if you have family members diagnosed with colorectal cancer or certain inflammatory bowel diseases like ulcerative colitis or Crohn's disease (especially over age 45), be aware that this could put you at greater risk - so take extra care!
Know the signs and symptoms
Some common signs and symptoms of colorectal cancer include:
- Feeling tired
- Having a change in weight
- Bloating/gas/constipation/diarrhea lasting more than 4 weeks
- Blood in your stool (which may look like black tarry stools)
- Rectal bleeding
If you have any of these symptoms that last more than 4 weeks, it is important to consult your family doctor or primary care physician.
Screenings play an important role in the detection of colorectal cancer
Talk with your doctor about which is the best colorectal cancer screening for you. Tests that are used to examine the inside of the large intestine (colon) and rectum, tests that can detect hidden blood in the stool, or screenings that can identify genetic changes in the cells of the colon could all be possibilities, depending on your age and other individual risk factors.
Take control of your colorectal health
Your family doctor or primary care physician can help you understand your risk factors and what you can do to protect yourself from colorectal cancer. They can also provide guidance on when you should get screened. Don't wait until something is wrong to see your doctor – make sure you stay on top of your colorectal health and get the peace of mind that comes with knowing you're doing everything you can to protect yourself.
To find a Redeemer Health family doctor or primary care physician, call 800-818-4747 or visit the Redeemer Health website.
categories:

Redeemer Health Support at Home received the distinguished 2023 Best of Home Care - Leader in Experience Award from HCP, the leading firm in experience management for home care. The Leader in Experience Award is the highest recognition awarded by HCP and is given to select home care businesses that consistently rank among the very highest in 10 or more quality metrics.
As a Leader in Experience, Redeemer Health Support at Home is now recognized among the 10% of home care providers participating in the nationwide HCP Experience Management Program. Both clients and caregivers were interviewed by HCP and they consistently offered high satisfaction ratings in areas such as caregiver training, compassion of caregivers, communication, scheduling, client/caregiver compatibility, and more.
Visit here to learn more about Redeemer Health Support at Home.
categories:

The extraordinary care delivered in the Senior Behavioral Health Unit (SBHU) at Holy Redeemer Hospital resulted in a donation from a grateful family. Their philanthropy, in turn, has brought music to patients' ears. The family of a former patient made it possible to stream music in all SBHU inpatient rooms. Now it's as easy as saying "play Frank Sinatra" and Fly Me to the Moon will fill a patient's room with magical melodies and memories.
Go no further than a quick Google search to find reams of research that support music's therapeutic benefits:
- It reduces anxiety and the physical effects of stress.
- It improves healing.
- It helps manage disease.
- It eases depression and other symptoms in the elderly.
- It helps improve self-expression and communication.
Music's profound effects on us are physical, psychological, cognitive and social. And now it's available in the SBHU space with a simple voice prompt. The goal of the installation was to enhance a patient's ability to be in an environment of their own choice, creating their own experiences and evoking meaningful memories. Said the grateful family about their donation: "(We) wish the music to bring a bit of peace in your soul and to comfort you."
Each patient room has been outfitted with ADA-compliant controls for music selection and volume, as well as integration with patient hearing aids. The common rooms in the unit also now have 60-inch televisions with Bluetooth headphones for patients.
